Why nutrition and strength training matter more than the number on the scales
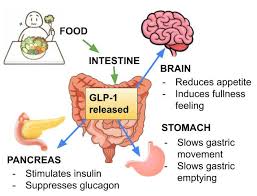
GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro) have changed the landscape of weight-loss treatment. For many people, losing 15–20% of body weight feels transformative.
However, for peri-menopausal women, GLP-1 medications can come with hidden risks—particularly when weight loss occurs without adequate nutrition and strength training support.
Key Takeaways
-
Up to 1 in 5 people using GLP-1 medications develop nutritional deficiencies within 12 months, with vitamin D and calcium most commonly affected
-
Appetite suppression often results in low protein intake, increasing the risk of muscle loss during peri-menopause
-
Standard multivitamins are rarely sufficient to meet calcium and vitamin D requirements
-
Resistance training and personalised nutrition planning are essential to protect muscle mass and bone density
GLP-1 Summary
The Promise — and the Paradox of GLP-1 Medications
GLP-1 medications work by slowing gastric emptying and reducing appetite. This makes it easier to eat less—but it also means people often consume far fewer nutrients overall.
Research shows total calorie intake can drop by 16–39% while taking GLP-1 medications. During peri-menopause—when declining oestrogen already increases the risk of osteoporosis and sarcopenia (muscle loss)—this reduction can be problematic.
Weight loss alone does not guarantee better health if muscle strength and bone density are being lost at the same time.
Nutritional Deficiencies Are More Common Than Expected
Large studies show that approximately 22% of GLP-1 users develop nutritional deficiencies within one year.
The most commonly affected nutrients include:
-
Vitamin D
-
Calcium
-
Protein
-
B-group vitamins
-
Zinc
Early symptoms may include fatigue, hair thinning, muscle weakness, poor concentration, low mood, or anxiety. Left unaddressed, these deficiencies can significantly increase the risk of falls, fractures, and long-term loss of independence in peri-menopausal women.
Why a Standard Multivitamin Isn’t Enough
Many women assume a daily multivitamin will protect them. Unfortunately, most products are designed for people eating normal calorie intakes, not those experiencing appetite suppression.
Typical multivitamins provide:
-
200–300 mg of calcium (well below the ~1,300 mg required)
-
400–800 IU of vitamin D, often insufficient for bone health
-
No potassium, despite its importance for muscle and nerve function
Without targeted planning, key nutrients can be missed entirely.

Steve Jeffries instructs a client through strength and conditioning training.
A Smarter Approach: Nutrition + Strength Training
For peri-menopausal women using GLP-1 medications, a proactive, structured approach is essential.
Protein
-
Aim for 1.2–1.6 g/kg of body weight per day
-
Spread protein intake across meals to maximise muscle retention
-
Combine with 2–3 resistance-training sessions per week
While all movement is beneficial, lifting progressively heavier weights provides the stimulus needed to preserve muscle mass and bone density. A physiotherapist can help design a safe, individualised gym program, particularly if pain, injury or confidence are barriers.
Calcium & Vitamin D
-
1,300 mg of calcium daily, ideally from food where possible
-
800–1,000 IU of vitamin D daily, or higher if blood levels are low
Omega-3 Fatty Acids
-
May support heart health, muscle recovery, and cognitive function, especially when total food intake is reduced
Why Weight Often Returns After Stopping GLP-1s
Many people are surprised when weight returns after stopping GLP-1 therapy. Studies suggest patients regain up to two-thirds of lost weight within 12 months.
This happens because medication does not address:
For peri-menopausal women, repeated cycles of weight loss and regain can worsen bone loss and muscle decline, increasing long-term injury risk.
The Role of an Accredited Practising Dietitian
Women who work with an Accredited Practising Dietitian during GLP-1 therapy consistently achieve better and more sustainable outcomes.
A dietitian can:
-
Create nutrient-dense meal plans that work with reduced appetite
-
Recommend targeted supplementation based on blood results
-
Manage GI side effects such as nausea or constipation
-
Build long-term eating strategies that continue after medication stops
The Bottom Line
GLP-1 medications can be powerful tools—but they are not a stand-alone solution.
For peri-menopausal women, the greatest risk is not failing to lose weight, but losing muscle strength, bone density, and long-term resilience along the way.
When GLP-1 therapy is combined with expert nutrition support, resistance training, and physiotherapy guidance, weight loss can support lasting health, independence, and quality of life.